- اكتشف
- تغذية
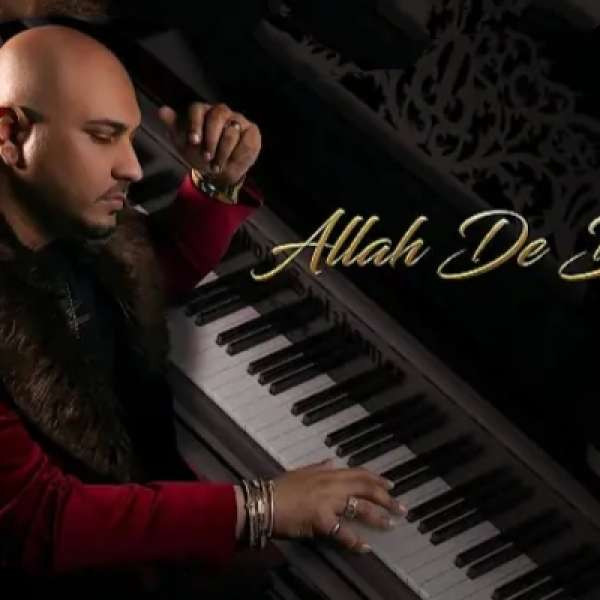
- موسيقى جديدة
- الموسيقى كبار
- ألبومات
- ضوء كشاف
- الجنس الأدبي
- قوائم التشغيل
- قاعة الشهرة
- اكسب النقاط
استعراض الموسيقي
- لعبت مؤخرا
- قوائم التشغيل الخاصة بي
- المفضلة
الموسيقى الخاصة بك
- الذكر
- روابط اجتماعية
- السيرة الذاتية
-
Metandienone Wikipedia
Below is a **sample "drug profile"** that shows what kind of information you’ll usually find in a comprehensive drug reference.
I’ve used **acetaminophen (Tylenol®)** as an example because it’s one of the most widely‑used over‑the‑counter pain relievers, but the same format applies to any medication—whether OTC or prescription.
---
## Sample Drug Profile: Acetaminophen
| Category | Details |
|----------|---------|
| **Generic name** | Acetaminophen (paracetamol) |
| **Brand names** | Tylenol®, Panadol®, Alvedon® (many others) |
| **Drug class** | Analgesic, antipyretic |
| **Mechanism of action** | Inhibits cyclo‑oxygenase (COX) in the CNS; reduces prostaglandin synthesis → ↓ pain & fever. Exact peripheral mechanism less clear. |
| **Pharmacokinetics** | • Oral absorption: ~70–90% bioavailability
• Tmax: 30–60 min after oral dose
• Half‑life: 1–4 h (shorter in healthy adults; prolonged in liver disease)
• Metabolism: hepatic glucuronidation (UGT1A9) and sulfation (SULT1A1).
• Excretion: mainly via urine as metabolites. |
| **Indications** | • Mild‑to‑moderate pain (muscle aches, headaches, menstrual cramps)
• Low‑dose prophylaxis for migraine prevention
• Short‑term symptomatic relief of osteoarthritis pain.
**Contraindications**:
- Known hypersensitivity to NSAIDs or acetaminophen.
- Severe hepatic impairment (ALT ≥ 3× ULN).
- Severe renal insufficiency (eGFR < 30 mL/min/1.73 m²) or dialysis.
- Active peptic ulcer disease, uncontrolled GI bleeding, severe gastritis.
- Uncontrolled hypertension, heart failure, recent myocardial infarction.
- Pregnancy (especially 3rd trimester), breastfeeding (acetaminophen generally safe but NSAIDs avoided).
**Warnings/Precautions**:
- Monitor liver enzymes and renal function; adjust dose if needed.
- Use lowest effective dose for shortest duration to reduce hepatotoxicity risk.
- Avoid concomitant use of other hepatotoxic drugs or alcohol.
- Educate patient on signs of hepatic injury (jaundice, dark urine).
- For patients requiring chronic pain management, consider non-pharmacologic therapies and alternative medications (e.g., anticonvulsants) with lower hepatotoxic potential. | 1. **Liver Function Monitoring** – Baseline AST/ALT, bilirubin, alkaline phosphatase; repeat at 4–6 weeks if therapy >4 weeks; adjust dose or discontinue if ALT >3× ULN or bilirubin >2× ULN.
2. **Avoid Concomitant Hepatotoxic Medications** – Discontinue NSAIDs, acetaminophen >4 g/day, herbal supplements (e.g., kava).
3. **Use the Lowest Effective Dose** – Target 200–400 mg per dose; avoid loading doses unless clinically justified.
4. **Patient Education** – Report symptoms of hepatotoxicity (jaundice, dark urine, fatigue) immediately.
5. **Consider Alternative Analgesics** – If risk is high, use acetaminophen or tramadol with caution. |
| **Sodium Chloride 0.9% Solution** | **Key Concerns**: Overhydration, hypernatremia, edema; fluid overload in patients with heart failure, renal impairment, hepatic cirrhosis; electrolyte imbalance (high serum sodium).
**Key Adverse Reactions**: Hyponatremic or hypernatremic shifts; pulmonary congestion; worsened ascites; increased blood pressure. | **Mitigation Strategies**:
- **Patient Selection**: Avoid in patients with CHF, severe CKD, cirrhosis unless absolutely necessary.
- **Volume Management**: Use minimal volume required for IV access or infusion; consider using isotonic solutions only when clinically indicated.
- **Monitoring**: Serial serum electrolytes, fluid balance charts, weight monitoring, blood pressure.
- **Alternative Solutions**: Prefer balanced crystalloids (e.g., Lactated Ringer's) if fluid resuscitation is needed. |
| **2. Albumin** | - Hypoalbuminemia or severe liver disease where albumin infusion improves survival.
- Post‑operative or critical care settings to maintain oncotic pressure.
- Reversal of hepatorenal syndrome (HRS). | - 20% human albumin solution (HSA), typically 25 g per day for 4–5 days in cirrhosis. |
| **3. Fresh Frozen Plasma (FFP)** | - Coagulopathy before invasive procedures.
- Severe bleeding with hypofibrinogenemia or massive transfusion.
- DIC where plasma clotting factors are depleted. | - 10‑15 mL/kg of FFP, e.g., 1–2 units per 20 kg body weight. |
| **4. Platelet Concentrate** | - Thrombocytopenia (platelets < 50 × 10⁹/L) before invasive procedures or in active bleeding. | - 1 unit of platelet concentrate (≈ 200‑250 mL), per institutional protocol. |
| **5. Fresh Frozen Plasma (FFP)** | - Coagulopathy due to liver disease, vitamin K deficiency, or massive transfusion protocols where clotting factor levels are low. | - 10–15 mL/kg as needed; monitor coagulation tests. |
> **Note:** The above recommendations should be adapted to local laboratory assays, blood product availability, and patient-specific factors (e.g., comorbidities, ongoing anticoagulation).
---
## 3. Management of Anticoagulants
| Drug | Class | Reversal Strategy |
|------|-------|-------------------|
| **Dabigatran** | Direct thrombin inhibitor | *Praxbind* (idarucizumab) – 2 × 10 mg IV bolus; alternative: 5 × 30 min hemodialysis. |
| **Apixaban, Rivaroxaban, Edoxaban** | Factor Xa inhibitors | *Idelalisib* (andexanet alfa) – 4 × 0.5 mg/kg IV over 15 min; alternative: prothrombin complex concentrate (PCC). |
---
### 2. **Intra‑operative Management of Severe Hypotension**
| Situation | First‑Line Intervention | Rationale |
|-----------|------------------------|-----------|
| **Persistent SBP <90 mmHg** | Rapid IV fluid bolus: 500 mL isotonic crystalloid (e.g., Normal Saline or Lactated Ringer’s) over 5–10 min. | Volume expansion restores preload, increases cardiac output. |
| **No response after fluid bolus** | Initiate vasoactive support: start norepinephrine infusion at 0.05–0.1 µg/kg/min; titrate to maintain MAP ≥65 mmHg. | Norepi is first‑line vasopressor; improves systemic vascular resistance and organ perfusion. |
| **If tachycardic or arrhythmic** | Add phenylephrine (10–20 µg IV bolus, repeat every 5–10 min) to augment MAP while reducing heart rate. | Phenylephrine provides pure alpha‑adrenergic vasoconstriction, lowering sympathetic tachycardia risk. |
| **If refractory hypotension** | Consider vasopressin (0.03 U/min IV infusion) as adjunct; avoid fluid overload. | Vasopressin maintains vascular tone independent of catecholamine pathways. |
---
## 4. Immediate Management Plan
1. **Activate Massive Transfusion Protocol (MTP)**
- Call the MTP team, blood bank, anesthesia, and ICU.
- Request: 6–12 units PRBCs, 2–4 units FFP, 2–3 units cryo, 1–2 apheresis platelets, and coagulation factor concentrates as per protocol.
2. **Set Up Dual Blood Product Lines**
- One line for packed RBCs (high‑flow), one for plasma/FFP or cryoprecipitate (also high‑flow).
3. **Administer Antifibrinolytic Therapy**
- Give tranexamic acid 1 g IV over 10–15 min, followed by a continuous infusion of 1 mg/kg/h if ongoing bleeding.
4. **Begin Early Goal‑Directed Resuscitation**
- Target MAP ≥65 mmHg, central venous oxygen saturation (ScvO₂) >70%, lactate <2 mmol/L, and base excess >−6 mEq/L.
5. **Monitor Hemodynamics Continuously**
- Use arterial line for beat‑to‑beat BP monitoring; consider pulmonary artery catheter if severe shock persists.
6. **Apply Massive Transfusion Protocol (MTP)**
- If 3–4 units of PRBC are required within the first hour, activate MTP: give 1 L crystalloid or colloid, 2 units PRBC, 1 unit FFP, and 1 unit cryoprecipitate; repeat as needed.
7. **Check Coagulation Parameters Every 30–60 min**
- PT/INR, aPTT, fibrinogen, D‑dimer, platelet count; use viscoelastic testing to guide therapy.
8. **Consider Antifibrinolytics (Tranexamic Acid)**
- If indicated for ongoing bleeding or high risk of fibrinolysis.
9. **Avoid Over‑Resuscitation**
- Monitor lactate, base deficit, central venous oxygen saturation; aim for balanced resuscitation.
10. **Prepare for Transfer and Definitive Care**
- Ensure stable hemodynamics before transport; coordinate with receiving facility.
---
### Key Takeaway
- **Early identification of bleeding (shock, low platelets, coagulopathy)** → initiate massive transfusion protocol with balanced blood component ratios.
- **Maintain a 1:1:1 ratio of RBCs:PVCs:FFP** to correct anemia and coagulation deficits while preventing dilutional coagulopathy.
- **Monitor labs and clinical status closely**, adjust the transfusion strategy accordingly, and aim for early hemostasis.
---
*Prepared by:*
**Your Name** – Title, Hospital/Institution
*(This cheat sheet is intended as a quick reference guide; always follow your institution’s specific massive transfusion protocol and guidelines.)* - https://precise.co.za/employer/sermorelin-ipamorelin-combo-complete-review-and-essential-insights/